Yes, Medicaid does cover prescription drugs, but the details of the coverage (and any copays you might owe) depend on where you live.
Remember that Medicaid is a state-run program, which means every state sets its own rules within federal guidelines, including what prescription drugs are covered.
Here’s how prescription coverage works under Medicaid, what costs you might see at the pharmacy, and why your state’s rules matter when it comes to prescription drug coverage.
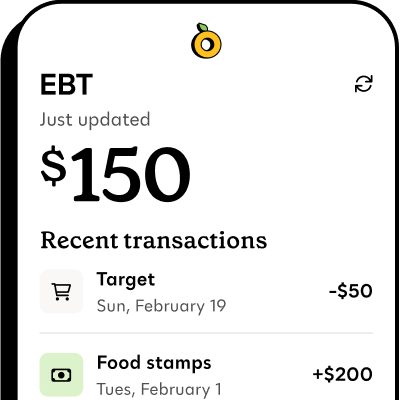
Propel is the #1-rated EBT balance checking app
Does Medicaid cover prescription drugs?#does-medicaid-cover-prescription-drugs
Prescription drug coverage is optional under federal Medicaid rules, but as of September 2025, all states cover prescriptions for people who qualify for Medicaid. That means you can fill most prescriptions using your Medicaid card at participating pharmacies.
Medicaid rules can change though, and Medicaid prescription drug coverage may look different in the future. You should double-check your state’s Medicaid website or ask your case worker if you’re unsure about current rules.
What prescriptions are covered by Medicaid?#what-prescriptions-are-covered-by-medicaid
Medicaid is run by each state, and often through private managed care plans. That’s why prescription coverage under Medicaid can look different depending on where you live and which health plan you have.
The exact list of covered prescription drugs that your state and your Medicaid health plan cover can be found on something called a formulary, which is basically a state-specific list of covered medicines.
What is a formulary for Medicaid?#what-is-a-formulary-for-medicaid
Every state Medicaid program, and often each managed care plan within the state, keeps a formulary. A formulary is a list of medicines that are covered by a health insurance plan. You’ll find two categories of medications on your formulary:
- Preferred drugs: These are the prescription medicines that Medicaid (or your specific plan) wants you to use first. They’re usually lower-cost or have been negotiated at a discount. If your doctor prescribes a preferred drug, you can usually get it filled right away without extra steps
- Non-preferred drugs/“require special approval”: These medicines may still be covered, but you’ll need approval from Medicaid. You usually don’t need to do anything extra to get approval—your doctor will explain to Medicaid (or your health plan) why you need that specific medicine instead of a preferred one. If approved, Medicaid will pay for it
If your prescription isn’t in your plan’s formulary, your doctor can submit something called a “prior authorization request” to try and get it covered. This is just a formal request to Medicaid.
What else affects whether a prescription is covered by Medicaid?#what-else-affects-whether-a-prescription-is-covered-by-medicaid
Some additional factors can affect what prescription drugs you can get with your Medicaid including:
- Managed care plans: Most people on Medicaid are enrolled in a managed care plan (MCO). These private health plans manage your prescription benefits, which means the formulary, pharmacies you can go to, and approval rules may be different depending on the plan
- Brand or generic: Most states and plans require the use of generics when available, unless your doctor shows that you have a medical need for a brand-name drug
- Limits: Some states or plans limit the number of prescriptions you can get per month. Some may require step therapy (trying a lower-cost medicine first before a more expensive one)
Do you have to pay copays for prescriptions with Medicaid?#do-you-have-to-pay-copays-for-prescriptions-with-medicaid
Most of the time, covered prescriptions are free (or at very low-cost) if you have Medicaid. According to federal Medicaid rules, total out-of-pocket costs for your household can’t go over 5% of your monthly or quarterly income.
This includes copays for visits and prescription drug costs. However, prescription drug copays are usually very low.
Exact costs vary by state and plan:
- Some states and managed care plans charge small copays, usually between $1 and $5 per prescription. Some states charge no copay at all for prescriptions
- Many groups (children, pregnant people, people in nursing homes) may pay no copay at all
- Managed care plans cannot charge more than what’s allowed under Medicaid law, but they may have different copay rules or preferred pharmacy networks
If your prescription isn’t covered by your Medicaid plan, you may have to:
- Work with your doctor to request prior authorization
- Switch to a different drug that’s covered
- Pay the full price
What to do if your prescription isn’t covered by Medicaid#what-to-do-if-your-prescription-isnt-covered-by-medicaid
If you find out your medication isn’t covered under your Medicaid plan:
- Request prior authorization: You can ask your doctor to send paperwork to Medicaid explaining why you need a specific medicine. Urgent requests can take between 24 to 72 hours, but standard requests may take up to 14 days for approval. If your request is denied, you might be able to appeal, but appeals can take up to 30 days
- Ask your doctor for a different medication: You can ask your doctor if there’s a generic or alternate medicine that is covered by your health plan
- Switch pharmacies: Most Medicaid plans only allow you to use certain pharmacies. If your medicine isn’t covered, you should check with your insurance to see if it is the prescription or the pharmacy that isn’t covered. If you need to, you can change pharmacies
Other ways to find free or low-cost prescription medications#other-ways-to-find-free-or-low-cost-prescription-medications
If your prior authorization is denied, and you can’t find a good alternative medication, you may be able to get help from a patient assistance program, nonprofit, or local community resource.
Here are some ways to get help if you’re having trouble affording prescriptions:
- Patient Assistance Programs: Many drug companies offer Patient Assistance Programs (PAPs) that provide certain medications for free or at a lower cost if you meet income guidelines. You can ask your doctor, pharmacist, or caseworker for help finding a PAP
- Community organizations: National nonprofits like NeedyMeds or the Partnership for Prescription Assistance can connect you with low-cost or free medication options. You can also dial 211 or visit 211.org to be connected to community organizations in your area that help with prescription costs, transportation to pharmacies, or other health-related needs
- State programs: You can ask your Medicaid caseworker if your state offers any special programs for prescriptions not covered by Medicaid