What is the Annual Enrollment Period (AEP) for Medicare?

If you have Medicaid or Medicare, you may have heard of the AEP, short for Annual Enrollment Period. The AEP is the period of time each year when you can review your Medicare health coverage plan and make changes if you need to.
- The AEP goes from October 15 to December 7 each year
- AEP is most often talked about for Medicare, but it also matters for anyone with dual eligibility (people who have both Medicaid and Medicare).
- Medicaid itself doesn’t have a standard annual enrollment period, but some states do have specific time periods when you can change your Medicaid health plan.
Here’s how the AEP works, how it affects people with Medicaid and Medicare, and when you can change plans
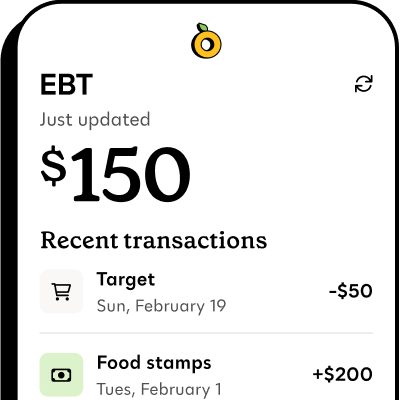
Propel is the #1-rated EBT balance checking app
What is the AEP for Medicare?#what-is-the-aep-for-medicare
Typically, once you enroll in Medicare, you’ll keep the same plan for the year unless it’s one of the official enrollment periods or you qualify for a special circumstance. Your plan determines which specific doctors, hospitals, or other healthcare providers you can see.
The Annual Enrollment Period (AEP) happens each year from October 15 to December 7—it’s when you can change your Medicare health plan without special circumstances. Changes take effect on January 1 of the upcoming year.
It is important to note that the Medicare AEP is different from the Medicare Advantage Open Enrollment Period, which runs from January 1 to March 31.
The Medicare Advantage Open Enrollment Period gives people with Medicare Advantage plans a second chance to change their plan if their chosen plan doesn’t meet their needs.
What can you do during AEP?#what-can-you-do-during-aep
During the AEP window (October 15 to December 7) Medicare recipients can:
- Look at your Medicare plan’s annual notice of changes to see what’s new for next year and decide if you want to change plans
- Switch from Original Medicare to a Medicare Advantage plan
- Switch from a Medicare Advantage plan to Original Medicare
- Change from one Medicare Advantage plan to another
- Join, switch, or drop a Part D prescription drug plan
Remember that Medicaid and Medicare cover different services. If you have both, this is your chance to make sure your Medicaid and Medicare coverage are working together in the best way for your needs.
What can’t you do during AEP?#what-cant-you-do-during-aep
The Annual Enrollment Period is a time to review, and if needed, change your Medicare plan.
The AEP is only for Medicare, not Medicaid, so you can’t change your Medicaid health insurance plan during this time unless you’re in a situation that qualifies you to change your Medicaid coverage.
The AEP is also not an application period—you can apply to Medicare or Medicaid year-round, any time. The AEP period does not impact Medicare applications or renewals.
Can you change Medicaid plans during AEP?#can-you-change-medicaid-plans-during-aep
The AEP is only for Medicare, not Medicaid, but Medicaid does have certain times where you can change plans.
Most states use Medicaid managed care plans, which means you may be able to change plans under certain conditions. However, unlike Medicare, Medicaid is a state-run program and does not have a national AEP.
Here’s when you can usually change Medicaid plans:
- When you first enroll: Depending on your state, you often have 30 to 90 days to change managed care plans after you’re approved for Medicaid
- During open enrollment periods: Some states hold annual or twice-a-year windows when you can change your Medicaid plan
- For “good cause”: You can usually request a change outside of Medicaid open enrollment if you have a good reason, like if your doctor no longer takes your insurance, you’ve moved to a new area, or you’re having issues with quality of care
Contact your case manager or a local Medicaid office to learn about your state’s Medicaid managed care enrollment period.